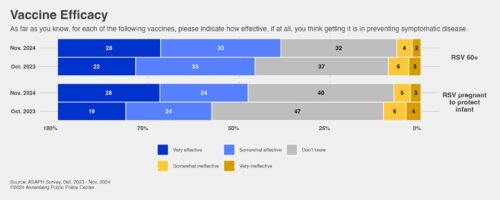
A year after becoming available, vaccines to protect against RSV in newborns and older adults are being more widely accepted by the American public, according to a new Annenberg Public Policy Center (APPC) health survey conducted in November 2024.
Over half of U.S. adults (52%) think the vaccine given to pregnant individuals to protect their infants from RSV (respiratory syncytial virus) is effective, up from 42% in October 2023, soon after the Centers for Disease Control and Prevention (CDC) recommended the vaccine. And 61% say the RSV vaccine for adults age 60 and older is effective, up from 54% in October 2023.
The rise in perceived effectiveness for the RSV vaccine comes even though there has been no sign to date of a dreaded “tripledemic,” the wave of flu, Covid-19, and RSV illnesses that filled emergency rooms in the fall and winter of 2022-23 and may have resulted in over 100,000 U.S. deaths. As of Dec. 20, 2024, the CDC reports overall moderate levels of acute respiratory illness, though flu season is underway with levels increasing across the country, Covid-19 activity is increasing from low levels in some areas of the country, and RSV activity is high and increasing in most U.S. areas, especially in young children.
The rise also comes as several of president-elect Donald Trump’s nominees for leading policy-making health positions have cast doubt on the efficacy and safety of vaccines, notably Health and Human Services Secretary nominee Robert F. Kennedy Jr., who has said “no vaccine” is safe and effective, and CDC chief nominee Dave Weldon, who, like Kennedy, has promoted the disproven link between vaccines and autism.
The APPC survey findings are based on a nationally representative panel survey of 1,771 U.S. adults fielded from Nov. 14-24, 2024, and has a margin of error of ± 3.3 percentage points. For more on the survey, see the end of this news release or the topline.
Vaccine hesitancy may have plateaued
The past several years have shown evidence of increased vaccine hesitancy. (See our October 2023 survey release, “Vaccine Confidence Falls as Belief in Health Misinformation Grows.”) However, by several measures in the November survey, including the RSV findings noted above, public acceptance of vaccination has risen slightly or held steady:
- 86% of respondents say the measles, mumps, and rubella vaccine (MMR) is safe, up from 81% in October 2023. The rebound brings it back toward the 88% who perceived it as safe in August 2022.
- 83% say the flu vaccine is safe, unchanged from October 2023.
- 65% say the Covid-19 vaccine is safe, unchanged from last fall.
- The perceived effectiveness of a variety of other vaccines is unchanged from October 2023.
- Over three-quarters of the public would recommend various vaccines, when appropriate, to members of their families and households.
In addition, despite continuing attacks on the safety and efficacy of certain vaccines by some politicians, 9 in 10 respondents say it is important for parents to get their children vaccinated: 72% say it is very or extremely important and 19% say it is somewhat important. Only 10% say it is not at all or not very important that parents get their children vaccinated.
Flu vaccine vs. Covid-19
In the survey, U.S. adults view the seasonal flu shot as more effective at reducing the risk of getting a severe case of the flu this season (75%) than the Covid booster is at reducing the risk of getting a severe case of Covid this season (55%). There’s been a significant increase in understanding that the flu shot doesn’t necessarily prevent a person who is exposed to the flu from getting sick but it does make the infection less severe (54%, up from 48% in October 2023). Fewer people say they are unsure what effect a flu shot has on a person who is later exposed to someone with the flu (14%, down from 20%).
The November data show that fewer people have received or plan to receive the Covid booster, as compared with the flu shot:
- Just over half of survey respondents (51%) either got the seasonal flu shot (40%) or say they are very likely to (11%) get it, compared with 38% who either got the latest Covid-19 booster (29%) or say they are very likely to (9%).
- The most common reason people select to explain why they have received the Covid booster and the flu shot is to protect themselves against catching that illness (82% and 78%, respectively).
- More people report getting the flu shot because they “get it every year” (76%) than those who report getting the Covid booster because they “get one every time a new booster comes out” (51%).
- 68% know they can get a Covid booster and a flu shot in the same visit to a health care clinic or pharmacy, unchanged from October 2023, though there’s a significant increase in the number who report that this is definitely true (44%, up from 38% in October 2023).
Flu knowledge
- Most people (80%) know the effectiveness of the seasonal flu shot varies year to year.
- Although most people (69%) see this year’s flu vaccine as effective at reducing the risk of getting the flu (unchanged from October 2023), more people think it is ineffective this fall (20%) than last fall (15%).
- In fact, early reports suggest that this seasonal flu vaccine may be less effective than last year’s: Based on reports from five South American countries, the CDC has said the effectiveness of the seasonal flu vaccine at cutting the risk of hospitalization among high-risk groups appears to be 35%, lower than the 51.9% seen in those countries last flu season, according to WebMD.
- 69% know that there is value in getting a flu shot after November, but 19% are unsure.
- Most people (80%) know it is possible to spread the flu to others even if you have no symptoms, up from 76% in January of 2023. (The CDC says that some “people can be infected with influenza viruses and have no symptoms but may still be able to spread the virus to their close contacts.”)
- Most (71%) know that the flu shot is the best defense against seasonal flu.
- However, only 42% believe that everyone 6 months of age and older should get a flu shot, unchanged from last year.
Beliefs in vaccine effectiveness and safety
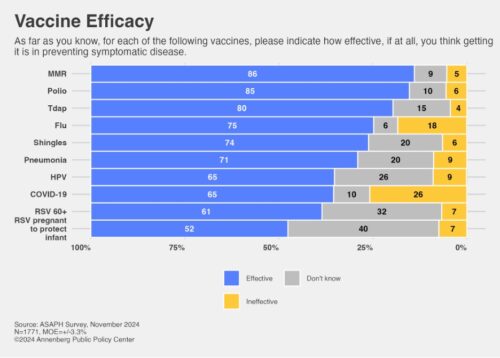
Longstanding vaccines such as the MMR, polio, and Tdap (tetanus, diphtheria, and pertussis) vaccines are usually top-rated by the public in effectiveness, safety, and in recommendations that others get the vaccines. Newer vaccines such as the Covid-19 vaccine or those for which public health advice has recently changed – such as the CDC recommendation that adults 50 and older get a vaccine against pneumonia – are less familiar and often lower-rated by the public.
Recommending vaccines. Here are the public’s views on recommending vaccines to others:
- MMR vaccine: 90% would be likely to recommend an MMR vaccine for a child in their household who is either between the ages of 12-15 months or 4 to 6 years old.
- Polio vaccine: 88% would be likely to recommend a polio vaccine to a child in their household of 2 to 6 months old.
- Tdap vaccine: 85% would be likely to recommend a Tdap vaccine to a child in their household of 11-12 years old or an adult in their family.
- Shingles vaccine: 82% would be likely to recommend a shingles vaccine to someone age 50+ in their family.
- HPV vaccine: 79% would be likely to recommend an HPV (human papillomavirus) vaccine for a child aged 11 or 12 years old in their household.
- Pneumonia vaccine: 77% would be likely to recommend a pneumonia vaccine to a person aged 50 or older in their family, down from 84% who were likely to recommend it to someone 65 or older in their family in April 2022. The CDC recommended lowering the age for the vaccine on Oct. 23, 2024, weeks before this survey was fielded.
Vaccine safety. Public views on vaccine safety:
- MMR: 86% say the MMR vaccine is safe, up from 81% in October 2023 (as noted above)
- Flu: 83% say the flu vaccine is safe, unchanged
- Covid-19: 65% say the Covid-19 vaccine is safe, unchanged from October 2023 but lower than 73% in August 2022.
Vaccine effectiveness. Public views on vaccine effectiveness are stable with the exception of RSV, which rose as noted above. The following percentages saw these vaccines as effective. Comparisons are to October 2023, if this question was asked then:
- MMR: 86% see the vaccine as effective (unchanged)
- Polio: 85%
- Tdap: 80%
- Flu: 75% (unchanged)
- Shingles: 74% (unchanged)
- Pneumonia: 71% (unchanged)
- HPV: 65% (unchanged)
- Covid-19: 65% (unchanged)
- RSV for adults 60 and older: 61%, up from 54% in October 2023
- RSV for pregnant individuals: 52%, up from 42% in October 2023
APPC’s Annenberg Science and Public Health knowledge survey
The survey data come from the 22nd wave of a nationally representative panel of 1,771 U.S. adults conducted for the Annenberg Public Policy Center by SSRS, an independent market research company. Most have been empaneled since April 2021. To account for attrition, small replenishment samples have been added over time using a random probability sampling design. The most recent replenishment, in September 2024, added 360 respondents to the sample. This wave of the Annenberg Science and Public Health Knowledge (ASAPH) survey was fielded Nov. 14-24, 2024. The margin of sampling error (MOE) is ± 3.3 percentage points at the 95% confidence level. All figures are rounded to the nearest whole number and may not add to 100%. Combined subcategories may not add to totals in the topline and text due to rounding.
Download the topline and the methods report.
The policy center has been tracking the American public’s knowledge, beliefs, and behaviors regarding vaccination, Covid-19, flu, RSV, and other consequential health issues through this survey panel over the past two-and-a-half years. In addition to APPC director Kathleen Hall Jamieson, APPC’s team on the survey includes research analysts Laura A. Gibson and Shawn Patterson Jr.; Patrick E. Jamieson, director of the Annenberg Health and Risk Communication Institute; and Ken Winneg, managing director of survey research.
The Annenberg Public Policy Center was established in 1993 to educate the public and policy makers about communication’s role in advancing public understanding of political, science, and health issues at the local, state, and federal levels. Find APPC on X, Facebook, and Threads.