Syphilis cases are on the rise around the globe, but many Americans don’t know the symptoms.
In January, the Centers for Disease Control and Prevention (CDC) reported that syphilis cases had risen 80 percent over the five years from 2018 to 2022, totaling more than 200,000 in 2022, the last year for which data are available.
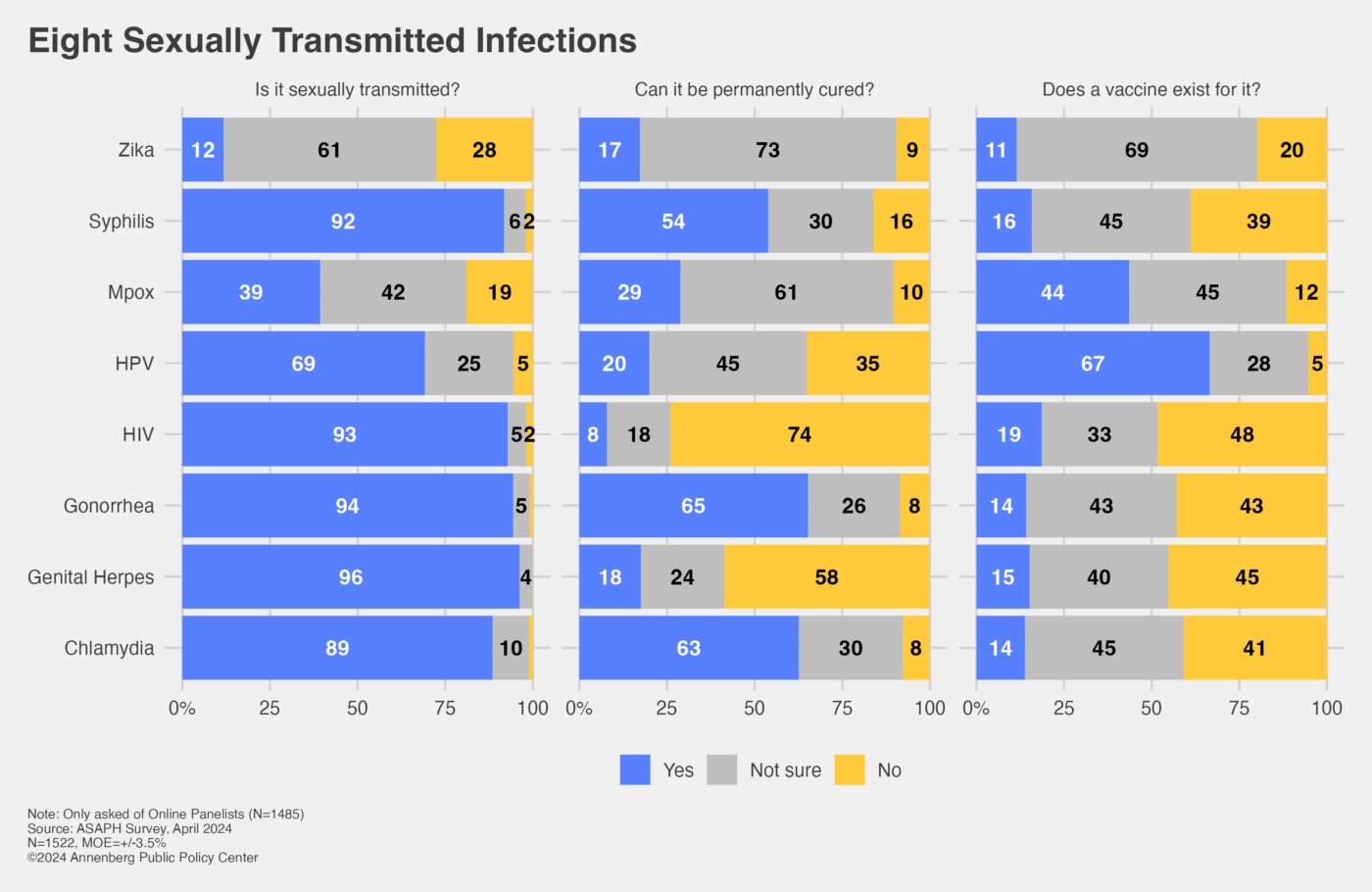
Yet just over half of U.S. adults (54%) know that a case of syphilis can be permanently cured and most either mistakenly think there is a vaccine to prevent it (16%) or are unsure (45%), according to the Annenberg Public Policy Center’s new survey findings on sexually transmitted infections (STIs). The survey of U.S. adults finds that many are familiar with some ways they can protect themselves from syphilis but lack familiarity with its symptoms and signs.
The survey also finds areas of uncertainty about other STIs, including whether they can be cured and whether vaccines exist. Only a third of the public knows that HPV (human papillomavirus) cannot be permanently cured and a third of the public does not know there is a vaccine to prevent it. (The CDC reports that the HPV vaccine has the potential to prevent more than 90% of HPV-attributable cancers.) Two years after a global outbreak of mpox, formerly called monkeypox, most people do not know whether it can be cured (it can be) or whether a vaccine exists (it does).
“With the rising number of syphilis cases, knowing the causes, symptoms, and treatment for it assumes added importance,” said Kathleen Hall Jamieson, director of the Annenberg Public Policy Center (APPC) of the University of Pennsylvania.
APPC’s latest Annenberg Science and Public Health (ASAPH) Knowledge survey, conducted from April 18-24, 2024, questioned a national probability sample of over 1,500 empaneled U.S. adults about their knowledge about sexually transmitted infections, with more extensive questions about knowledge and treatment of syphilis and HIV. See the survey toplines.
Protecting oneself from contracting syphilis
What people do know: When asked to select which, among the following, are ways that individuals can protect themselves from contracting syphilis, most people got the answers right – selecting the correct ways and skipping the wrong answers:
- 78% correctly chose abstinence, or not engaging in sex
- 77% correctly chose using a condom
- 94% correctly did NOT select oral contraception (the pill)
- 89% correctly did NOT select wearing a diaphragm
- 78% correctly did NOT choose getting a vaccine (there is none)
But 71% did not select using only clean needles, which is one of the ways to protect oneself from contracting syphilis.
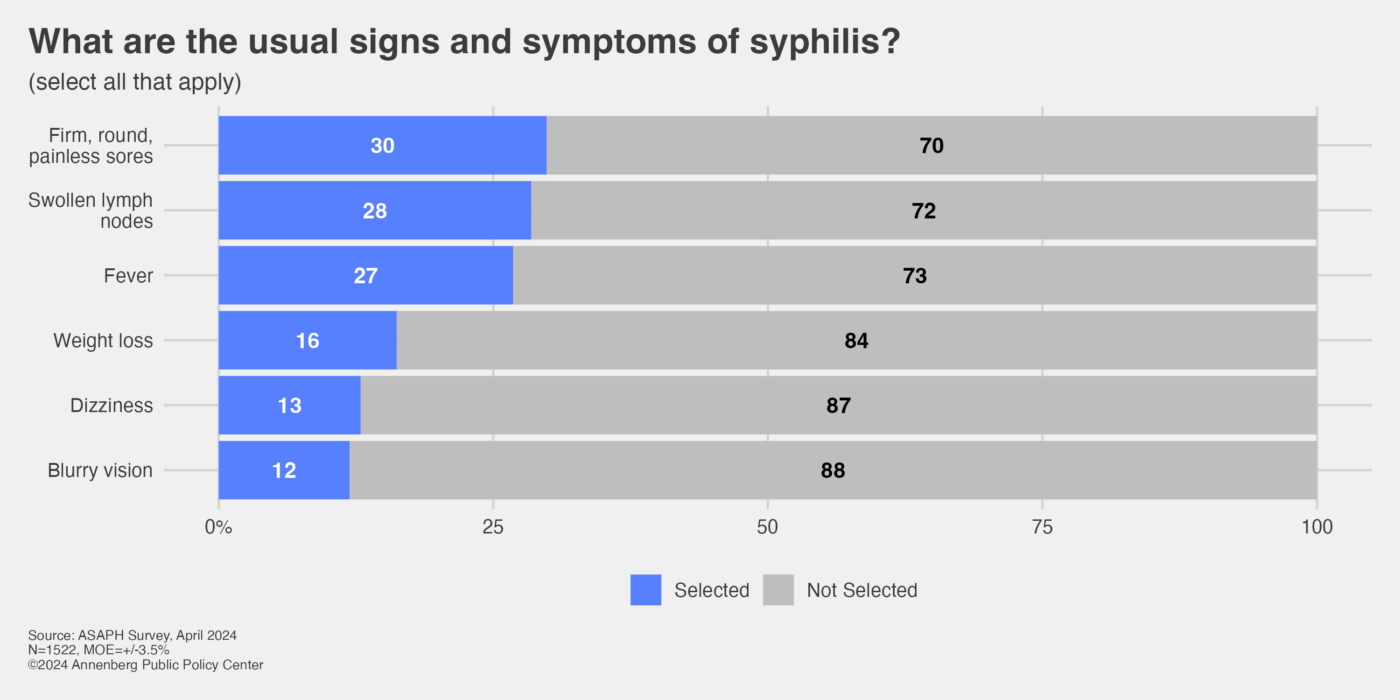
Failing to recognize symptoms of syphilis
What people don’t know: When asked to select usual syphilis signs and symptoms from a list, less than a third of survey respondents selected any of these symptoms (according to the CDC, all are symptoms of types of syphilis):
- 30% selected “firm, round, painless sores”
- 28% selected “swollen lymph nodes”
- 27% selected “fever”
- 16% selected “weight loss”
- 13% selected “dizziness or lightheadedness” [the CDC says it’s a sign of otosyphilis]
- 12% selected “blurry vision” [the CDC says it’s a sign of ocular syphilis]
How can HIV be spread?
The survey finds that U.S. adults are generally knowledgeable about how HIV (human immunodeficiency virus) can be spread. Asked to select from a list which of these methods are ways in which HIV can be spread:
- 95% know HIV can be spread through unprotected sex
- 90% know HIV can be spread by sharing needles
- 67% know HIV can be spread from an infected person to their child while giving birth
Respondents also know that the following means are not ways in which HIV can be spread:
- 89% correctly did NOT select by exposure to airborne droplets that are coughed or sneezed into the air by an infected person.
- 88% correctly did NOT select from touching a surface contaminated by the virus
- 85% correctly did NOT select by using the “party drugs” known as poppers
However, only 1 in 3 adults (33%) knows that HIV can also be spread from an infected parent breastfeeding a child.
How can you get an STI?
The survey finds that U.S. adults are generally familiar with how you can get an STI. Asked to select from which of the following activities you can get an STI:
- 98% know you can get it from vaginal sex
- 89% know you can get it from oral sex
- 93% know you can get it from anal sex
- 91% know you can get it from genital-to-genital contact
In addition, 44% selected kissing as a way to get an STI (generally not, but it may be a risk factor for oral gonorrhea) and 21% chose sitting on a toilet (which is not a form of transmission).
Can it be cured and is there a vaccine?
Large majorities of the public know that six out of eight infections considered in the survey are sexually transmitted infections, including syphilis, HPV, HIV, gonorrhea, genital herpes, and chlamydia – with the exceptions being mpox (which 39% identified as sexually transmitted) and Zika (which 12% identified as sexually transmitted). Zika is a mosquito-borne infection that also can be sexually transmitted. Although mpox cases have declined since the 2022 outbreak, “low-level [U.S.] transmission continued,” according to public health officials, who in June urged continuing vigilance, especially among men who have sex with men.
The public is not sure whether some of the STI infections can be permanently cured or whether a vaccine exists to prevent them. Over half know that gonorrhea (65%), chlamydia (63%) and syphilis (54%) can be cured, but under a third (29%) know that mpox can be cured. But:
- 91% are not sure whether Zika can be cured or think it can be (it can’t be cured)
- 65% are not sure whether HPV can be cured or think it can be (it can’t be cured)
- 42% are not sure whether genital herpes can be cured or think it can be (it can’t be cured)
- 26% are not sure whether HIV can be cured or think it can be (it can’t be cured)
Asked whether a vaccine exists to prevent these infections, only for HPV is a majority of the public aware (67%) that there is one, while 44% knows there is a vaccine for mpox. For these other infections there is no vaccine and most of the public is either not sure or incorrect:
- Zika: 80% do not know there’s no vaccine (69% not sure, 11% say yes there is)
- Syphilis: 61% do not know there’s no vaccine (45% not sure, 16% yes)
- HIV: 52% do not know there’s no vaccine (33% not sure, 19% yes)
- Gonorrhea: 57% do not know there’s no vaccine (43% not sure, 14% yes)
- Genital herpes: 55% do not know there’s no vaccine (40% not sure, 15% yes)
- Chlamydia: 59% do not know there’s no vaccine (45% not sure, 14% yes)
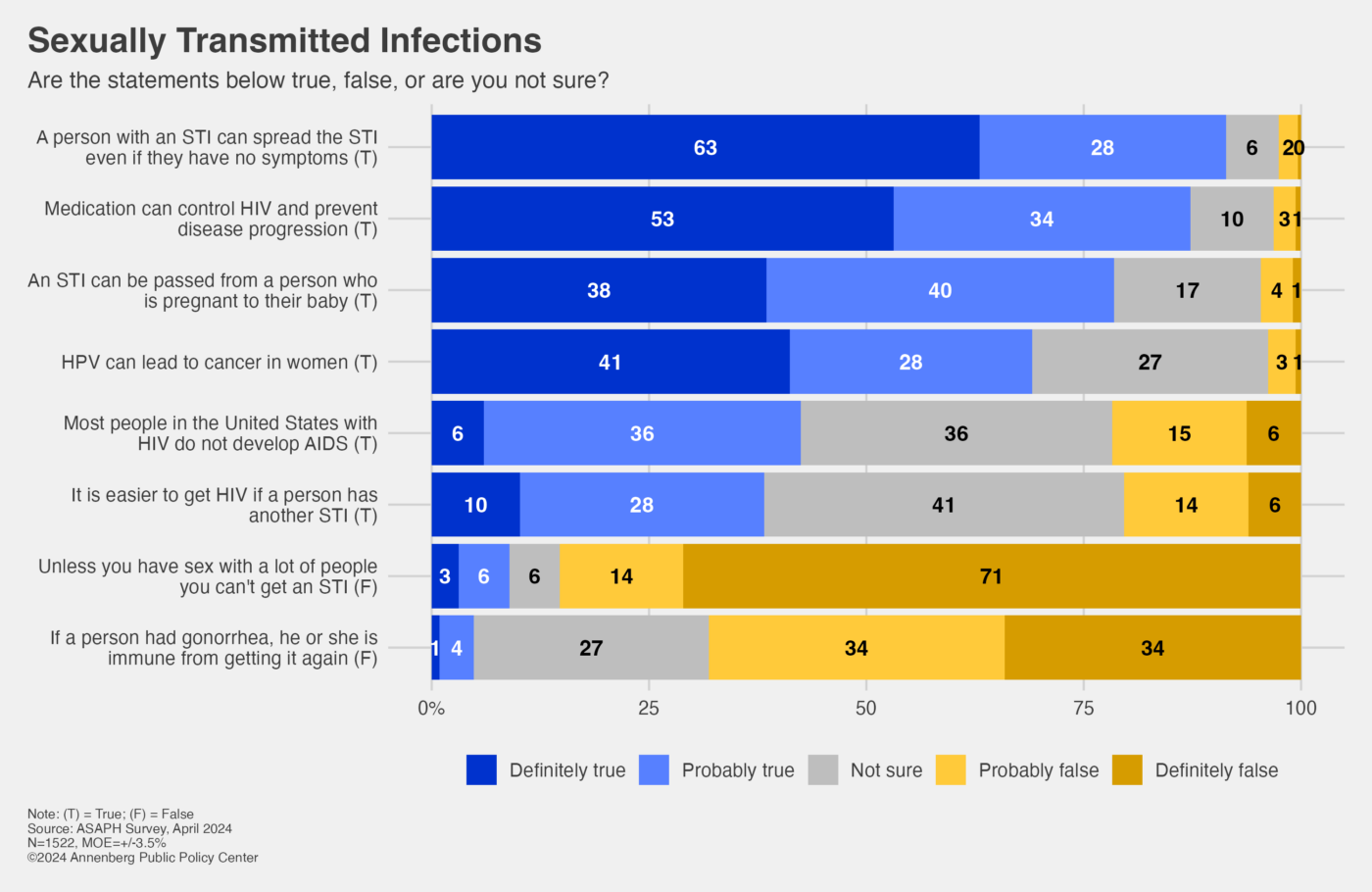
Other knowledge about STIs
Much of the public does have a reasonable level of background knowledge about STIs. Large majorities know that someone with an STI can spread the STI to others even if there are no symptoms (91% true); that medication can control HIV and prevent disease progression (87% true); that an STI can be passed from a person who is pregnant to their baby (78% true); and that HPV can lead to cancer in women (69%). And they know it is false to say that unless you have sex with a lot of people you can’t get an STI (85% false) and that it is false to say that if a person had gonorrhea he or she is immune from getting it again (68% false).
The questions with the greatest uncertainty involve HIV. Just 42% know that most people in the United States with HIV do not develop AIDS (36% not sure) and 38% know it is easier to get HIV if a person has another STI (41% not sure).
APPC’s ASAPH survey
The survey data come from the 19th wave of a nationally representative panel of 1,522 U.S. adults, first empaneled in April 2021, conducted for the Annenberg Public Policy Center by SSRS, an independent market research company. This wave of the Annenberg Science and Public Health Knowledge (ASAPH) survey was fielded April 18-24, 2024, and has a margin of sampling error (MOE) of ± 3.5 percentage points at the 95% confidence level. All figures are rounded to the nearest whole number and may not add to 100%. Combined subcategories may not add to totals in the topline and text due to rounding.
Download the toplines and methodology statement.
The policy center has been tracking the American public’s knowledge, beliefs, and behaviors regarding vaccination, Covid-19, flu, maternal health, climate change, and other consequential health issues through this survey panel for over three years. In addition to Jamieson, the APPC team includes Shawn Patterson Jr., who analyzed the data; Patrick E. Jamieson, director of the Annenberg Health and Risk Communication Institute, who developed the questions; and Ken Winneg, managing director of survey research, who supervised the fielding of the survey.